It’s a Thursday afternoon in early December, and the waiting room of SPARCC Sports Medicine, Rehabilitation and Concussion Center is packed with people. Patients cycle in and out of the expansive exercise room, undergoing tests for exertion, balance and cognitive capabilities alongside athletic trainers and clinical technicians. After each patient completes his or her testing, they’re ushered into a room where results and progress will be reviewed by one of SPARCC’s practitioners.
Unlike most doctor’s offices and despite the high volume of patients, visits at SPARCC are never quick. Some appointments last upward of two hours.
That’s because, according to one of SPARCC’s founders, there’s no “cookbook blueprint” for sports injuries — and particularly concussions.
“Our vision was not to have folks think about a doctor’s appointment, but to be an all-encompassing experience for that patient,” said Dr. Mo Mortazavi. “We feel very privileged to be in a model where we don’t feel rushed and we don’t have to limit your care because we need to see a quota of patients.”
‘The right fit for the right community’

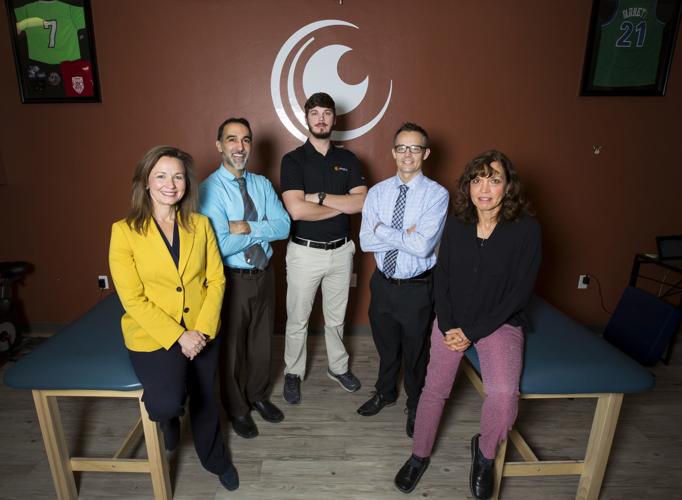
From left, Dr. Tanya Polec, neuro-optometric rehabilitation specialist; Dr. Mo Mortazavi, pediatric sports medicine physician; Gaige Braden, certified athletic trainer; Dr. Jonathan Minor, pediatric non-operative sports medicine physician; and Leslie Streeter, nurse practitioner, devise a multistep recovery plan for each of their patients with brain injuries.
SPARCC, which was created in 2016, is open to patients of all ages and activity levels. It’s also Tucson’s only certified youth sports medicine specialists and Southern Arizona’s only comprehensive concussion care center.
SPARCC is the brainchild of Mortazavi and software engineer Andrew Zelinski, who met while playing football together at UC Davis. The two partnered up to form SPARCC after seeing a need and opportunity in Tucson.
“It was the right fit for the right community,” Mortazavi said, adding that the practice takes the “village approach” of collaborative treatment in dealing with its patients and operates on a rehabilitation and education-based philosophy.
Mortazavi began working with Tucson Unified School District about five years ago to develop the evidence-based Return to Learn program for concussion management. Shortly thereafter, he was appointed TUSD’s medical director, a position he maintains as he continues to hold monthly meetings with district administrators and employees, including athletic department workers and school nurses. The Amphitheater and Vail school districts followed suit, adopting the Return to Learn program.
SPARCC initially operated out of multiple locations across town with no insurance contracts, but quickly became the go-to concussion treatment center in town, given Mortazavi’s specialization in comprehensive concussion management.
“I was basically seeing patients for free,” Mortazavi said. “Just to get the word out, and also there was a lot of passion for this, because it was evolving with what we were doing. That was really fun.”
A year later, SPARCC had grown and was contracted by multiple insurers and offering transparent rates for self-payers and information about what insurance companies would cover in terms of services. The practice, still operating out of multiple locations, brought in a new practitioner, Dr. Jon Minor, to specialize in running and dance medicine.
In 2018, SPARCC found a permanent home on Fairness Drive, close to Tucson Medical Center. Later that year, the practice added nurse practitioner Leslie Streeter to specialize in concussions, musculoskeletal injuries and health issues affecting female athletes. While the clinic has no shortage of concussion patients, sprains, strains, fractures and growth plate injuries and overload are a huge part of SPARCC’s business, Mortazavi said.
Minor is the only pediatric nonoperative sports medicine doctor in town, which allows SPARCC to focus on pediatric overuse injuries, which Mortazavi said is an epidemic in and of itself with how hard kids are being pushed to perform in sports.
“We recognized the community’s need and we wanted to go that extra mile,” Zelinski said. “It took years to run efficiently, but the vision was there and we knew what the kids’ needed.”
Because of the different backgrounds in medicine and sports, the SPARCC team complements one other well, Mortazavi said.
Despite SPARCC’s unconventional tendency toward lengthy appointments, the clinic’s practitioners still see about 100 traumatic brain injury patients per week, and up to 40 on a busy day. Mortazavi sees the bulk of the patients with concussions and traumatic brain injuries, visiting with up to 60 a week and sometimes as many as 20 per day.
“Our philosophy is really taking that time, even if it’s an hour with a patient, to make sure that they really understand what their diagnosis is and why they need to do what they need to do,” Mortazavi said.
Mortazavi said that there’s no set timeline for recovering from a brain injury, but the increasing science surrounding concussions has provided an ever-growing toolbox for assessing and treating patients. Advanced tools such as cognitive impact testing, oculomotor trackers and voltage testing assist Mortazavi in planning and monitoring a patient’s recovery.
“The history and exam is central to everything that we do, but these tools act as an aid for us and can give us this extra layer of protection,” Mortazavi said.

Dr. Mo Mortazavi, pediatric sports medicine physician, pose for a portrait at SPARCC Sports Medicine Rehabilitation and Concussion Care, 5199 E Farness Dr., in Tucson, Ariz. on December 18th, 2019. SPARCC, a sports medicine clinic, has quickly become the go-to spot for young athletes who are recovering from concussions and other sports-related injuries.
Mortazavi initiates a multistep recovery plan with every concussion or traumatic brain injury patient that he sees, meeting each patient where they’re at in terms of tolerance to exercise. SPARCC’s clinic has a quiet room for patients with brain injuries so problematic that most wouldn’t think to exercise them. In the quiet room, patients can use a recumbent bike at a very low intensity and duration. The room has low or no lighting and a blank wall to reduce outside stimulus.
“When you take away the risks, they can exercise a little bit every day,” Mortazavi said, adding that there’s a difference between clearing a patient to exercise and clearing he or she to return to sports.
The general exercise room is much larger, and the focal part of the clinic, set up with a treadmill, standard exercise bike, weights and various exam tables and other pieces of equipment. Multiple patients can cycle through the room at the same time, working with a member of SPARCC’s 20-person core team, made up of clinical technicians, researchers, and various patient care specialists.
Studies have shown that the earlier a patient starts exercising, the faster his or her recovery time, Mortazavi said. Exercise also benefits mood, sleep and cognitive issues.
“It’s a matter of getting the right dose on board early,” Mortazavi said.
Increasing the patient’s tolerance to exercise isn’t the only component of a patient’s recovery process at SPARCC: Mortazavi and staffers also do work with balance and visual issues, which are common.
Every patient receives an individualized cognitive action plan, or ICAP, at the end of each visit to guide the recovery process.
While 75% of SPARCC’s patients are athletes, the clinic’s doors are open to patients with brain injuries involving non-athletes, such as car accidents, assaults and domestic violence victims. The injury is the same as in athletes and should be managed the same way, Mortazavi said.
“Nobody else does what we do the way that we do it,” Mortazavi said. “We’re not in a field where (our patients) come and see us once and we don’t see them again. We see our patients grow up. Whether its an ankle sprain that they come back for or another concussion, unfortunately that’s the nature of sports. Most of our families and our kids we have longstanding relationships with.”
Trouble ‘zeroing in’

University of Arizona lacrosse player Brynn Doyle, 23, runs through an exercise during a visit to SPARCC located on 5199 E. Farness Drive suite 101, on Dec. 12, 2019. Doyle is visiting the facility while recovering from a concussion.
Brynn Doyle, 23, was running next to a teammate during lacrosse practice at the University of Arizona a few months ago when she was hit in the lower jaw by a ball and knocked down.
Doyle said after her concussion was diagnosed, she started going to Campus Health for treatment, but there was no plan.
“They weren’t really zeroing in on the problem at Campus Health,” Doyle said during an interview at SPARCC earlier this month.
After several weeks, Doyle was struggling with classes and having issues with light sensitivity. Her mother searched the internet for concussion specialists, and found SPARCC. Doyle began treatments about a month ago, and quickly noticed an improvement, with her symptoms steadily decreasing as time passed.
Doyle is in the final step of her recovery plan, working at maximum precontact exertion in the SPARCC clinic during her visit in early December. Doyle said that she tried to go to lacrosse practice one time after the injury, but the bright lights and activity on the field proved to be too difficult.
During her visit to SPARCC earlier this month, Doyle did interval work on the treadmill followed by several floor exercises and tests of her balance and body’s response to exertion.
Doyle laughed, slightly out of breath, as she ran through the exercises, her candy-cane striped fingernails clenched tightly into fists at her side.
Later in her appointment, Doyle performed exercises to strengthen eye pairing and decrease double-vision with SPARCC’s athletic trainer, Gaige Braden.
Doyle, a public health major, said she likes the structure and regimen that “Dr. Mo” and the staff at SPARCC provided in her recovery plan. She’s eager to return to the field when the lacrosse season begins in January, or at least return to practice with her teammates.
‘It was heartbreaking’

Gabe Lopez, 14, a football player and wrestler at Cienega High School has an oculomotor scan performed on him during a visit to SPARCC located on 5199 E. Farness Drive suite 101, on Dec. 12, 2019. Lopez suffered a concussion during football practice and has been visiting the facility during his recovery.
Gabe Lopez was playing linebacker during Cienega High School football practice when he noticed an offensive tackle running toward him.
Lopez, 14, said because the tackle was a “big guy,” he didn’t think he would be able to catch him, but he was wrong.
The larger player caught up to Lopez, colliding with him in a helmet-to-helmet hit that Lopez said left him “trying to figure out where to stand.”
With a game on the schedule two days later in which Lopez expected to get a lot of playing time, he didn’t tell his coach about the hit. After an all-day headache the next day, he went Cienega’s athletic trainer and was diagnosed with a concussion.
Lopez’s symptoms included headaches, balance issues, noise and light sensitivity and sleep disturbances. After about a week, his mother, Deserie, noticed her son wasn’t improving, and he was also having difficulty finding the right words when he spoke.
“It was heartbreaking,” Deserie Lopez said. “He would start to stutter and then just stop talking.”
Deserie Lopez took Gabe to his pediatrician, who recommended that he start treatment at SPARCC immediately. Gabe Lopez was in the clinic the next day.
Then, on Halloween, Gabe’s 12-year-old brother, Tony, was waiting at parent pickup at Old Vail Middle School when he was hit in the temple with a rock and knocked out cold. Tony Lopez’s immediate symptoms included blurred vision and nausea, and the next day he was diagnosed with a concussion. Deserie Lopez knew where to go this time.
“One good thing about all this is that because the boys can’t watch TV, we’ve been playing a lot of board and card games,” Deserie Lopez said, adding that the whole family quit watching TV in solidarity with the boys. “We’ve had a lot more family time.”
Gabe and Tony’s father reads them game updates from his phone. Tony Lopez, a voracious reader, has been keeping up with his classmates by listening to “A Christmas Carol” on audiobook. Before his injury, Gabe Lopez had just gotten a high-energy Labrador retriever puppy. As part of his recovery, Gabe has been unable to exercise, meaning the whole family has been pitching in with puppy care.

University of Arizona lacrosse player Brynn Doyle, 23, has her blood pressure taken during her visit at SPARCC located on 5199 E. Farness Drive suite 101, on Dec. 12, 2019. In the background, 14-year-old Gabe Lopez runs an exertion test on the treadmill.
The biggest struggle has been limiting the boys’ physical activity, Deserie said. Tony Lopez loves PE so much that he signed up for two classes at school.
Gabe Lopez used to referee his younger brother’s flag football games, in addition to playing football himself, but now he tracks the games instead of officiating. Gabe has also has been watching wrestling practices at Cienega while waiting to be cleared to participate. He has been unable to participate in weights and ROTC drills, too.
That’s been the hardest part of recovery, he said.
“I’m getting behind and I can’t do the stuff I want to do,” Gabe Lopez said at SPARCC on a Thursday in December. “I’m not used to just sitting around talking to people.”
Gabe Lopez’s symptoms are improving, and he’s now in the final step of his recovery. While it’s unlikely he’ll be able to compete in wrestling matches next season, Deserie Lopez is hopeful that her son will be able to participate in drills with his teammates. Gabe Lopez has loftier goals, saying he wants to join the school’s rugby team in the spring and return to football in the fall, adding that there’s probably a place for him on the junior varsity team.
Deserie Lopez, sitting outside of her son’s field of vision, vehemently shakes her head back and forth.
“I think we’re done with football,” she said. It’s clear from Gabe’s smile that this conversation is far from over.
Deserie Lopez said she loves to see how much time the staff at SPARCC spends with her sons during their visits, adding that the staff has also helped the boys receive accommodations at school to address their concussion symptoms.
Mortazavi said that his work with TUSD changed the way he practiced medicine, alerting him to the need to fully explain a student’s recovery needs to school staff. The student’s ICAP feeds directly into his or her Return to Learn plan, which Mortazavi said is one of the hallmarks of SPARCC’s specialized treatment, along with active rehab.
“They really go above and beyond to help you and help your kids succeed,” Deserie said.